Medical Case Profiles
1.800.858.7378npic@oregonstate.edu
We're open from 8:00AM to 12:00PM Pacific Time, Mon-Fri
A to Z
Medical Case Profiles
Medical Cases and Topics for Health Care Providers are based upon inquiries received by NPIC, as well as relevant publications in the scientific literature. They areintended to educate health care providers about pesticide toxicology.
Using DEET Safely
Scenario:
An adult female presents to her primary care provider approximately 24 hours after a weekend camping trip. She is experiencing pain and redness in the antecubital fossa of her left arm. She does not report any known history of trauma or insect bites. Upon further history, it is learned that she had applied an insect repellent containing 50% DEET to exposed areas of the skin including the neck, arms, and lower extremities. She had used lower concentrations of DEET repellents in the past, with no reported history of adverse skin reactions. On this occasion, the insect repellent was applied approximately 18 hours prior to the onset of symptoms. She reports that she did not wash the treated skin at the end of the day. She does not report applying sunscreen or taking any medications prior to the onset of the rash. No other unusual exposures are reported.
Upon examination, a well-demarcated area of erythema is apparent in the left antecubital fossa. It is warm and tender to palpation. There are no other abnormal findings on physical examination. Upon re-evaluation 48 hours later, hemorrhagic blisters form in the erythematous area. Two days later the bullae spontaneously rupture, leaving a shallow ulceration which resolves over the course of the next 10 days.
Discussion:
Figure 1: DEET
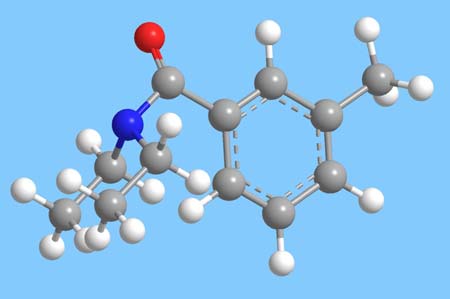
DEET (chemical name N,N-diethyl-3-methylbenzamide, former nomenclature N,N-diethyl-m-toluamide-Figure 1) is a widely utilized active ingredient in insect repellents. It was first developed for use by military personnel in 1946. Adverse skin reactions associated with DEET have been infrequently reported in the medical literature. Some case studies of military personnel have described similar bullous reactions occurring in healthy adults. Consistent findings in these reports include the use of repellents with a high concentration of DEET (greater than 50%), and the onset of an erythemtaous rash within 24 hours of application in certain treated areas of the skin (including the antecubital fossa and other regions where the skin may be occluded or covered by clothing during sleep).1,2
In several reported cases the erythema becomes a bullous eruption that subsequently ruptures, leaving an ulceration. In one case series, standard 48 hour patch testing with a dilute formulation of DEET (5%) was not effective in confirming the diagnosis, although under skin occlusion conditions with a 75% DEET formulation a similar constellation of skin findings was observed in some individuals.1 No other abnormal signs or symptoms were reported in these cases. While the results of these case series are suggestive of an irritant contact dermatitis from repellents containing a high concentration of DEET,1 case reports of immediate hypersensitivity reactions in association with the dermal application of DEET have also been infrequently reported in the medical literature.3,4
Based upon reviews of the epidemiological data on human exposures to DEET, the incidence of adverse effects from normal use is rare when compared to the widespread use of DEET by the general population.5,6,7 The EPA estimates that 38% of the U.S. population uses DEET each year. When adverse effects have been reported in association with the dermal application of DEET, the skin has been the organ system most frequently affected.5 Cases of transient eye irritation have also been frequently reported, resulting from accidental ocular exposures.5 Rare reports of more serious outcomes, including neurological symptoms and seizures, have been described in some cases. Many of these cases have been reported in association with the accidental or intentional ingestion of DEET, as well as overuse of repellent formulations.8,9
In 1998, the U.S. EPA conducted a re-registration eligibility decision for repellents containing DEET as active ingredient. The Agency and the EPA Scientific Advisory Panel reviewed toxicological data and incidents of adverse effects including neurological outcomes in humans, and determined that it was not possible to conclude whether reports of seizures were directly related to DEET exposure.10,11 The Agency concluded that the normal use of DEET does not present a health concern to the general population, and that improvements in label instructions were warranted to enhance the safety of their use and to minimize unnecessary exposure.11 Of relevance to this medical case profile, the labeling of DEET repellents directs users to wash treated skin with soap and water after returning indoors, and to not use repellents underneath clothing. Additional directions required on DEET repellent labels include:
- Read and follow all directions and precautions on this product label.
- Do not apply over cuts, wounds, or irritated skin.
- Do not apply to hands or near eyes and mouth of young children.
- Do not allow young children to apply this product.
- Use just enough repellent to cover exposed skin and/or clothing.
- Do not use under clothing.
- Avoid over-application of this product.
- Wash treated clothing before wearing it again.
- Use of this product may cause skin reactions in rare cases.
- For aerosol and pump spray formulations: Do not spray in enclosed areas.
- For aerosol and pump spray formulations: To apply to face, spray on hands first and then rub on face. Do not spray directly onto face.
This medical case profile is an example of the importance of understanding the pesticide label and complying with the labeling instructions. Health care providers can play an important role in reducing risks by understanding the pesticide label, incorporating compliance with labeling instructions into the exposure history, and ensuring that patients are using insect repellents safely. Other authorities, including the American Academy of Pediatrics and the Centers for Disease Control and Prevention, consider DEET to be the most effective insect repellent available and have provided additional guidelines to minimize risks and use DEET safely. These guidelines include selecting the lowest concentration of DEET that would be effective for the amount of time spent outdoors. For individuals who will be outdoors for two hours or less, a repellent containing less than 10% DEET will likely provide effective protection from mosquito bites. Repellents containing 20% DEET will provide effective protection for approximately four hours.12
References:
- Lamberg SI, 1. Mulrennan JA, Jr. Bullous reaction to diethyl toluamide (DEET). Resembling a blistering insect eruption. Arch Dermatol. 1969; 100:582-586
- Reuveni H, Yagupsky P. Diethyltoluamide-containing insect repellent: adverse effects in worldwide use. Arch Dermatol. 1982; 118:582-583
- Maibach HI, Johnson HL. Contact urticaria syndrome. Contact urticaria to diethyltoluamide (immediate-type hypersensitivity). Arch Dermatol. 1975; 111:726-730
- Miller JD. Anaphylaxis associated with insect repellent. N Engl J Med. 1982; 307:1341-1342
- Bell JW, Veltri JC, Page BC. Human Exposures to N,N-diethyl-m-toluamide insect repellents reported to the American Association of Poison Control Centers 1993-1997. Int J Toxicol. 2002; 21:341-352
- Koren G, Matsui D, Bailey B. DEET-based insect repellents: safety implications for children and pregnant and lactating women. CMAJ. 2003; 169:209-212
- Veltri JC, Osimitz TG, Bradford DC et al. Retrospective analysis of calls to poison control centers resulting from exposure to the insect repellent N,N-diethyl-m-toluamide (DEET) from 1985-1989. J Toxicol Clin Toxicol. 1994; 32:1-16
- Hampers LC, Oker E, Leikin JB. Topical use of DEET insect repellent as a cause of severe encephalopathy in a healthy adult male. Acad Emerg Med. 1999; 6:1295-1297
- Tenenbein M. Severe toxic reactions and death following the ingestion of diethyltoluamide-containing insect repellents. JAMA. 1987; 258:1509-1511
- FIFRA Scientific Advisory Panel. Scientific Advisory Panel meeting, June 4, 1997. 28-30. 6-4-1997. https://archive.epa.gov/scipoly/sap/meetings/web/html/hazard.html
- United States Environmental Protection Agency, Office of Prevention Pesticides and Toxic Substances. Reregistration Eligibility Decision: DEET. EPA738-R-98-010, 1-118. 1998. Washington, D.C. https://archive.epa.gov/pesticides/reregistration/web/pdf/0002red.pdf
- Fradin MS, Day JF. Comparative efficacy of insect repellents against mosquito bites. N Engl J Med. 2002; 347:13-18

